DVT and flying? What’s the risk and what’s the likelihood of that happening to you? Unfortunately, the answer isn’t simple and clear cut. DVT and flying is frequently referred to as the “economy class syndrome”. That’s because of the tight, cramped stiff seats that are frequently found on most airplanes. However, DVTs can occur in any seat and any class. Deep vein thrombosis went unrecognized for decades because the clots that formed in the large veins in the legs often started coming off in little pieces after a person had been home for a day or two. DVT sufferers would go to the emergency room with a suspected possible heart attack that was actually a DVT.
1DVT and Flying – It’s the Sitting!
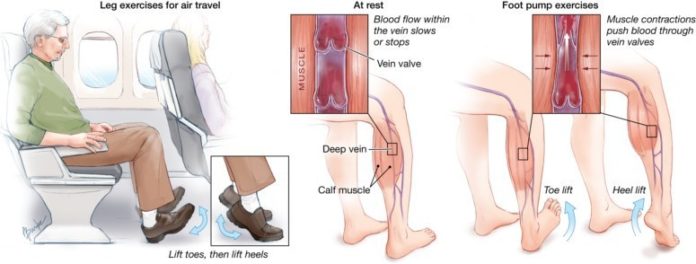
No matter what the mode of transportation, sitting motionless for long periods may put some travelers at an increased risk for deep vein thrombosis (DVT), which is a blood clot blood in a vein deep within the muscles, usually located in the thigh or calf. But people can reduce their risk of getting DVT, says the American Heart Association (AHA), by taking some simple precautions prior to going on long flights or trips. The AHA estimates that 1 out of every 1,000 Americans develops a DVT each year. However, anyone traveling more than four hours, whether by air, car, bus, or train, can be at risk for blood clots.
People who fly four hours or more, a recent study found, have three times the risk of developing clots compared with periods of time when they did not travel recent studies have shown. The longer the flight, the more at risk you are for developing a clot. Flights lasting 8-10 hours or longer pose the greatest risk.
In some cases, the DVT will dissolve and go away on its own. However, in more serious cases, it can cause pain, swelling and warmth of the affected leg. Or it can break off and travel to the blood vessels of your lungs, causing pulmonary embolism (PE).
Your level of risk depends on the duration of travel as well as whether you have any other risks for blood clots. Most people who develop travel-associated blood clots have one or more other risks for blood clots, such as:
- Older age (risk increases after age 40)
- Obesity
- Recent surgery or injury (within 3 months)
- Use of estrogen-containing contraceptives
- Hormone replacement therapy
- Pregnancy and the postpartum period which is up to 6 weeks after childbirth
- Previous blood clot or a family history of blood clots
- Active cancer or recent cancer treatment
- Limited mobility – can be from various reasons such as a leg in a cast
- Catheter placed in a large vein
- Varicose veins
The combination of long-distance travel with one or more of these risks may increase the likelihood of developing a blood clot. The more risks you have, the greater your chances of experiencing a blood clot. If you plan on traveling soon, talk with your doctor to learn more about what you can do to protect your health. The most important thing you can do is to learn and recognize the symptoms of blood clots.